4 low-dose strengths for accurate pediatric dosing
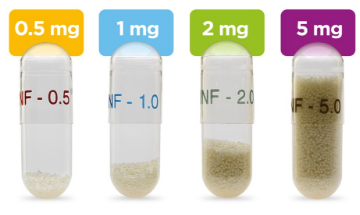
ALKINDI SPRINKLE® (hydrocortisone) oral granules are stored in color-coded capsules for easy identification to help provide accurate dosing for children with adrenal insufficiency.
- Available in 4 flexible dosage strengths: 0.5 mg, 1 mg, 2 mg, and 5 mg
- Less than 0.8 mm in size, much smaller than the FDA-recommended size to prevent choking1
- Granules are uniform in size and shape1
- Stored in easy-to-open capsules
ALKINDI SPRINKLE is for oral use only and should be removed from the capsule prior to taking. The capsule can be a choking hazard for small children.
How ALKINDI SPRINKLE works:
Unlike hydrocortisone treatments for adults, the various strengths of ALKINDI SPRINKLE can be individualized to your child’s specific cortisol need for the lowest possible dose without having to crush or split tablets.
If your child doesn’t get the entire dose of ALKINDI SPRINKLE because of vomiting or spitting out some of the granules, contact your doctor to see if another dose is needed.
Accurate hydrocortisone dosing can provide safe and effective treatment in children with adrenal insufficiency
Dosing accuracy in children with adrenal insufficiency is essential.2 If a child gets too much (overdosing) or too little (underdosing) hydrocortisone, they may experience poor health outcomes that can last for years, even into their adult years.3-6
Overdosing can lead to long-term health problems
If your child gets more hydrocortisone than prescribed, they are at risk for long-term health problems that could last into adulthood.2
- Growth failure5
- Abnormal weight gain5
- Cushing’s syndrome4
- High blood pressure3-5
Underdosing can lead to short-term health problems
If your child gets less hydrocortisone than prescribed, they could be in immediate danger.2
- Adrenal crisis5
- Masculine features in some conditions causing adrenal insufficiency or congenital adrenal hyperplasia (CAH)5
- Rapid growth in some conditions causing adrenal insufficiency or CAH4,5
- Poor response to stress6
- Weight loss5,6
No representation is made regarding the use of ALKINDI SPRINKLE in relation to these conditions.

Managing cortisol levels in newborns and children with adrenal insufficiency requires accurate dosing
ALKINDI SPRINKLE was made specifically for children with adrenal insufficiency
Accurately treat your child with the dose your doctor prescribed.
ALKINDI SPRINKLE hydrocortisone oral granules are small enough to sprinkle onto soft food or directly into your child’s mouth. The capsules are designed to be opened and the medicine given on a full or empty stomach with a sip of fluids to ensure all granules are swallowed. The 4 color-coded strengths can be individualized to your child’s specific cortisol need for the lowest possible dose without crushing or splitting tablets.
Always give ALKINDI SPRINKLE exactly as prescribed by your doctor.
On a spoon with food
Pour all granules onto a spoonful of soft food, like yogurt or applesauce, and give within 5 minutes.
Directly into your child’s mouth
Pour all granules of the prescribed dose directly into your child’s mouth.
If your child doesn’t get the entire dose of ALKINDI SPRINKLE because of vomiting or spitting out some of the granules, contact your doctor to see if another dose is needed.
Administering ALKINDI SPRINKLE
-

Check expiration and prepare
Check the expiration date on the ALKINDI SPRINKLE bottle. Do not use after the expiration date listed on the bottle.
Then, remove the prescribed dose of ALKINDI SPRINKLE capsules from the bottle. -

Hold and tap
Hold capsule with the writing at the top. Tap the capsule to make sure the granules fall to the bottom.
-

Squeeze
Gently squeeze the bottom of the capsule to loosen the top from the bottom.
-

Twist and remove
Carefully twist off the top of the capsule.
-

Sprinkle
ALKINDI SPRINKLE can be given by spoon with soft food or sprinkled directly into your child’s mouth.
-

Tap
Tap the capsule to ensure all the granules are removed. Avoid wetting the capsule on the tongue or soft food as this may result in granules remaining in the capsule.
-

Give fluids
After giving ALKINDI SPRINKLE, give your child a sip of fluids, such as water, milk, breast milk, or formula, right away to ensure all granules are swallowed.
ALKINDI SPRINKLE granules may sometimes be seen in stools because the center of the granule is not absorbed in the gut after the drug has been released.
ALKINDI SPRINKLE has a texture that may be new to your child
Some children may object to the texture of ALKINDI SPRINKLE in their mouth. It’s best to give with soft food, like yogurt or applesauce. Watch a short video of an actual family living with adrenal insufficiency administering ALKINDI SPRINKLE.
No pill splitting
No pill crushing
No compounding
Just sprinkles
ALKINDI SPRINKLE patient support is available through Eton Cares
Eton Cares is a dedicated support team available to answer your questions and help you reach your treatment goals.
References: 1. Center for Drug Evaluation and Research. Guidance for industry: size of beads in drug products labeled for sprinkle. Published May 2012. Accessed February 7, 2023. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/size-beads-drug-products-labeled-sprinkle-rev1 2. Neumann U, Whitaker MJ, Wiegand S, et al. Absorption and tolerability of taste-masked hydrocortisone granules in neonates, infants and children under 6 years of age with adrenal insufficiency. Clin Endocrinol (Oxf). 2018;88(1):21-29. doi:10.1111/cen.13447 3. Han TS, Conway GS, Willis DS, et al. Relationship between final height and health outcomes in adults with congenital adrenal hyperplasia: United Kingdom congenital adrenal hyperplasia adult study executive (CaHASE). J Clin Endocrinol Metab. 2014;99:E1547‐E1555. 4. Oprea A, Bonnet NCG, Pollé O, Lysy PA. Novel insights into glucocorticoid replacement therapy for pediatric and adult adrenal insufficiency. Ther Adv Endocrinol Metab. 2019;10:2042018818821294. doi:10.1177/2042018818821294 5. Bornstein SR, Allolio B, Arlt W, et al. Diagnosis and treatment of primary adrenal insufficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(2):364-389. doi:10.1210/ jc.2015-1710 6. Debono M, Newell Price J, Ross RJ. Novel strategies for hydrocortisone replacement. Best Pract Res Clin Endocrinol Metab. 2009;23(2):221-232. doi:10.1016/j.beem.2008.09.010

